CuraPatient
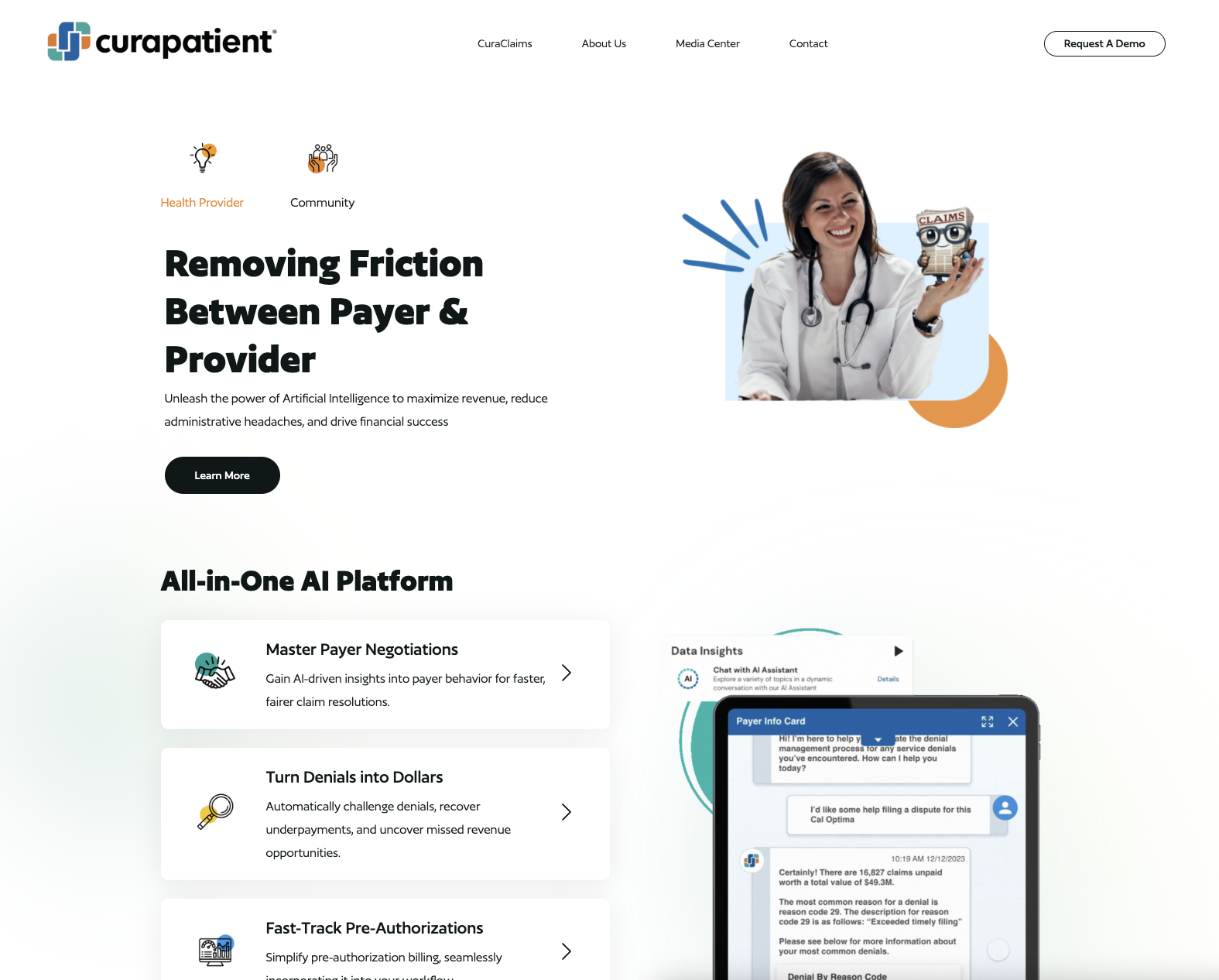
Enterprise AIAI-powered healthcare technology platform transforming payer-provider collaboration through automated claims processing, clinical documentation, and administrative workflow optimization.
CuraPatient company profile
Overview
CuraPatient stands as a transformative force in healthcare technology, leveraging artificial intelligence to bridge the critical gaps between payers and providers. Founded in 2014 and based in Irvine, California, the company has evolved into a comprehensive AI-powered platform that addresses some of healthcare’s most pressing administrative challenges.
With a mission to transform payer-provider collaboration through AI-powered solutions, CuraPatient has demonstrated remarkable impact during critical healthcare moments, including supporting the COVID-19 response by administering 1.3 million vaccinations in just six months and onboarding over 12,000 healthcare providers to their platform.
The company’s vision of “unlocking the potential of AI to shape the future of healthcare” drives their development of solutions that not only improve operational efficiency but also enhance patient outcomes through streamlined administrative processes.
AI-Powered Platform
CuraClaims Core Technology
CuraPatient’s flagship platform, CuraClaims, represents a sophisticated AI-driven approach to healthcare claims management:
Workflow Automation Orchestration: Intelligent automation that manages complex claims processing workflows, reducing manual intervention and processing time while maintaining accuracy and compliance standards.
Transparent Claims Valuation: Advanced AI algorithms that provide clear, explainable valuations for medical claims, enabling providers to understand reimbursement decisions and optimize their billing practices.
Regulatory Analysis Engine: Comprehensive analysis of contracts, procedures, and healthcare regulations to ensure compliance and identify optimization opportunities.
Advanced AI Capabilities
| AI Feature | Functionality | Healthcare Benefit | Impact |
|---|---|---|---|
| Automated Claims Processing | AI-driven claims review and validation | Reduced processing time and errors | 90% faster claims processing |
| Clinical Documentation AI | Intelligent medical record optimization | Improved coding accuracy | Enhanced reimbursement rates |
| Denial Prediction | Proactive identification of claim risks | Preventive claim management | Reduced denial rates |
| Revenue Recovery | AI-powered denial challenge system | Maximized revenue recovery | Increased collections efficiency |
Intuitive Dashboard Systems
Provider Analytics: Comprehensive dashboards that provide healthcare providers with actionable insights into their claims performance, denial patterns, and revenue optimization opportunities.
Real-Time Monitoring: Live tracking of claims status, processing bottlenecks, and system performance metrics to enable proactive management.
Predictive Insights: AI-powered forecasting that helps providers anticipate cash flow, identify potential issues, and optimize their revenue cycle management.
Healthcare Solutions
Claims Management Excellence
Pre-Authorization Intelligence: Automated pre-authorization processes that leverage AI to determine approval likelihood and streamline the authorization workflow.
Denial Challenge Automation: Sophisticated systems that automatically identify, analyze, and challenge inappropriate claim denials, maximizing revenue recovery.
Contract Analysis: AI-powered review of payer contracts to identify optimization opportunities and ensure maximum reimbursement rates.
Clinical Documentation Optimization
AI-Enhanced Documentation: Intelligent systems that help healthcare providers create more accurate and comprehensive clinical documentation, improving both patient care and reimbursement outcomes.
Coding Optimization: Advanced algorithms that suggest optimal medical coding to ensure accurate billing and maximum appropriate reimbursement.
Compliance Monitoring: Continuous monitoring of documentation practices to ensure adherence to healthcare regulations and standards.
Security and Compliance
Enterprise-Grade Security
CuraPatient has established itself as a leader in healthcare data security with comprehensive compliance certifications:
FedRAMP High Certification: Achieved FedRAMP High Certification Ready status, demonstrating the highest levels of security controls required for federal healthcare data.
NIST Security Framework: Implementation of 421 NIST security controls, providing comprehensive protection across all system components.
HIPAA Compliance: 100% HIPAA compliant operations ensuring patient data privacy and security at every level of the platform.
Data Protection Standards
End-to-End Encryption: Advanced encryption protocols that protect healthcare data during transmission and storage.
Access Controls: Sophisticated identity and access management systems that ensure only authorized personnel can access sensitive healthcare information.
Audit and Monitoring: Comprehensive logging and monitoring systems that provide complete audit trails for compliance and security oversight.
Market Impact
COVID-19 Response Leadership
CuraPatient demonstrated exceptional adaptability and impact during the COVID-19 pandemic:
Vaccination Program Support: Successfully administered 1.3 million vaccinations in six months, showcasing the platform’s scalability and reliability during crisis situations.
Student Health Screening: Supported 800,000 students with health screenings and testing, enabling safe return to educational environments.
Rapid Provider Onboarding: Quickly onboarded 12,000+ healthcare providers, demonstrating the platform’s ability to scale rapidly during increased demand.
Healthcare Industry Transformation
Administrative Efficiency: Significantly reducing administrative burdens on healthcare providers, allowing them to focus more resources on patient care.
Revenue Optimization: Helping healthcare organizations maximize their revenue through improved claims processing and denial management.
Payer-Provider Collaboration: Creating more transparent and efficient relationships between healthcare payers and providers through AI-powered insights.
Competitive Advantages
Regulatory Expertise: Deep understanding of healthcare regulations and compliance requirements built into every platform feature.
Proven Scalability: Demonstrated ability to rapidly scale operations during high-demand periods while maintaining quality and security.
Industry Recognition: FedRAMP certification and successful pandemic response have established CuraPatient as a trusted healthcare technology partner.
CuraPatient’s comprehensive approach to healthcare AI, combined with their proven track record and robust security framework, positions them as a critical technology partner for healthcare organizations seeking to optimize their operations while maintaining the highest standards of patient data protection and regulatory compliance.
